What is Hidradenitis Suppurativa (HS)?
This article has been provided as a valuable resource by MyHSTeam, a social support network of 15,000+ people with HS. Advanced Dermatology and Cosmetic Surgery treats HS and also offers clinical trials through our Ameriderm Research Division.
About HS:
- HS is a skin disease that causes painful, recurring bumps that may leak fluid and scar when they heal.
- Early diagnosis and treatment can benefit people with HS, but diagnosis is often delayed by years.
- HS is not contagious or caused by poor hygiene, but due to problems with the immune system.
- A dermatologist usually diagnoses HS.
- HS is not rare – millions of Americans and approximately 1 percent of the European population are believed to have HS.1
- Although HS cannot be cured, it can be effectively treated and may become inactive for long periods.
Between 1 and 4 percent of the population – an estimated 3.2 to 13 million Americans – live with hidradenitis suppurativa (HS), a skin condition characterized by painful bumps and sores in the skin.2 HS bumps may last for months, heal and recur repeatedly, form scars, or burst and leak foul-smelling pus. HS, also known as acne inversa, acne ectopica, apocrine acne, Verneuil’s disease, or fox den disease, can have a negative effect on the quality of life and often proves difficult to treat.1, 3, 4
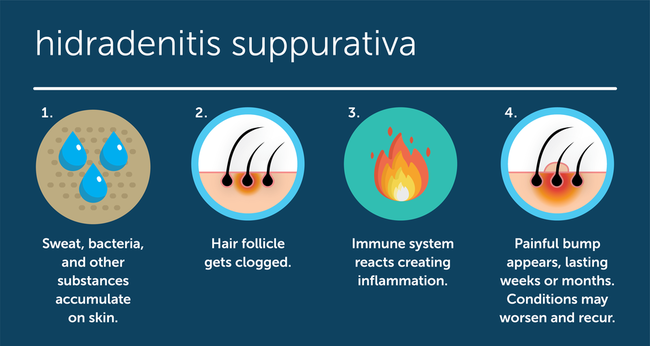
Hidradenitis suppurativa is often mistaken for other skin conditions including acne, boils, cysts, and folliculitis. Like acne, HS forms when the hair follicles clog with bacteria and other substances. However, HS is caused by a problem in the immune system rather than a blocked pore or an infection. Because HS can look like common skin conditions, it is best to see a dermatologist for diagnosis.5
HS can occur at any age but often develops between the ages of 20 and 30. It is more common in women than in men by a ratio of three to one.6 Early diagnosis and treatment can help manage HS symptoms, prevent progression, and avoid complications such as scarring. Unfortunately, there is an average seven-year delay in diagnosis.7 Depression and self-imposed isolation are common among people with HS, as the pain and visible effects on the skin take an emotional toll.8
What Causes Hidradenitis Suppurativa?
Hidradenitis suppurativa is a chronic inflammatory skin condition brought on by irregularities in the immune system.9 Some researchers believe that HS develops when the immune system overreacts to a plugged hair follicle.10
Where Does HS Occur?
Skin contains two types of sweat glands. Eccrine sweat glands release fluid onto the surface of the skin, and apocrine sweat glands release fluid into the hair follicles. HS is limited to parts of the skin containing apocrine sweat glands.11

Women tend to develop HS more commonly in the armpits, groin, and under the breasts.11 Men more commonly develop HS in the skin around the anus.11 In some people, the nape of the neck and the skin behind the ears can be affected as well.2
What Are the Symptoms of HS?
The disease usually starts with a single, painful bump that persists for weeks or months. Some people only experience mild symptoms, but for others, HS gets progressively worse.11
Symptoms of HS can include double-headed blackheads, as well as red and tender bumps or lesions that may grow larger. Hard, pea-sized lumps often mistaken for boils can also develop under the skin and persist for months.12
Swollen lumps associated with HS may spontaneously rupture with a foul-smelling discharge, and may heal and then recur. Lesions sometimes fuse into dermal abscesses. These abscesses may leak pus and can be hard to heal. Fistulas can also form, leading to the development of extensive tunnels under the skin known as sinus tracts.7
Sinus tracts can become linked under the skin’s surface, causing inflammation and allowing infection to travel deeper and become more widespread. In severe cases, thick, painful scar tissue can form and may limit body movement in affected areas.12
Some people with HS also experience itching, burning, and profuse sweating.13
HS can impact the quality of life by causing psychological symptoms such as depression, anxiety, stress, low self-esteem, social isolation, and problems with intimacy.14
Who Is at Risk for Hidradenitis Suppurativa?
Hidradenitis suppurativa affects between 1 and 4 percent of the global population.2 HS is three times more common in women than in men.6 People of African and European descent have a higher risk of developing HS, while it is rare among those of Asian background.11
In the U.S., African-American women aged 40 and under have the highest risk of developing hidradenitis suppurativa in comparison to other ethnic and age groups.7
HS usually begins around puberty when hormone levels rise and activate the apocrine sweat glands.10 Few people develop HS before 11 years of age, and if they do, it is often a case of early puberty.10 Developing HS after menopause or 55 years of age is rare.10

Genetics play a role in the development of hidradenitis suppurativa. About one-third of people who develop HS have a blood relative with the condition.10
Tobacco use may be a risk factor for developing hidradenitis suppurativa. While the connection requires further research, there is evidence that HS is more common among smokers than nonsmokers. A study of 50 million Americans found that smokers were almost twice as likely to be diagnosed with HS than nonsmokers. Other studies have found a relationship between smoking and greater HS severity.15
Obesity or being overweight may not be direct causes of HS, however they are associated with more severe symptoms. A study of 115 people with hidradenitis suppurativa found that people with a body mass index (BMI) considered obese had more severe symptoms than those without. Individuals with an overweight BMI had more severe symptoms than those with a normal BMI.16
HS seems more common in people with acne, and may be more common in women with polycystic ovary syndrome (PCOS).11
Common Myths About HS
There are many common misconceptions about hidradenitis suppurativa that contribute to stigma around this painful and sometimes debilitating condition. Here’s the truth behind several of the most common myths.
MYTH: HS is contagious
HS cannot be spread from one person to another. It is believed to be caused by a malfunctioning immune system.17
MYTH: HS is caused by a sexually-transmitted disease (STD)
HS is not contagious and is not caused by any type of infection. HS lesions often develop around the genitals and anus because these areas contain apocrine glands.
MYTH: HS is caused by poor hygiene
Dermatologists have determined that HS is not caused by poor hygiene.10 HS is caused by a malfunction with the immune system and may start with an immune reaction to a plugged hair follicle.10
MYTH: HS is a rare disease
According to the Centers for Disease Control and Prevention (CDC), a rare disease is one that affects fewer than 200,000 Americans.18 HS is not a rare disease, as it affects between 1 and 4 percent of the population, or 3.2 to 13 million Americans.2
What Are the Stages of HS?
Dermatologists describe cases of hidradenitis suppurativa from mild to severe using a system known as Hurley stages.2 Mild cases can consist of small bumps on the skin, blackheads, or a few skin cysts.5 More severe forms can lead to recurrent abscesses, which sometimes release foul-smelling fluid.5
The three Hurley stages are defined by the following symptoms:
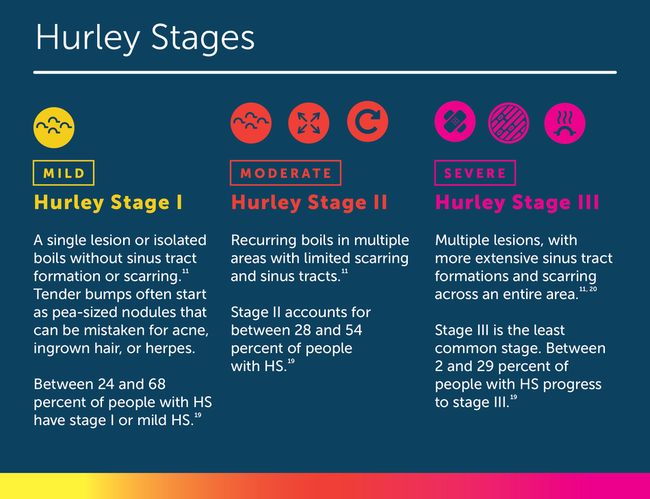
Some doctors also use the modified Sartorius score, designed in 2003. It was the first validated HS-dedicated tool and is based on four clinical parameters including which parts of the body are involved, the number and type of lesions, and the distance between lesions. The Sartorius score is used more for research than in daily clinical practice.20
Not all cases of hidradenitis suppurativa progress to more advanced stages, but some cases of HS can continue to reappear and grow more severe if not properly managed. Diagnosing and properly managing HS as early as possible is important to avoid progressing to a more severe stage.3
What Are the Treatment Options for HS?
There is currently no permanent cure for hidradenitis suppurativa, although it may become inactive for long periods after successful treatment.21
Medications, which may include antibiotics, corticosteroids, hormonal treatments, and certain biologics, improve symptoms in some people with HS. Some medications for HS are taken orally, while others are applied topically or injected. Antibiotics can reduce inflammation, fight infection, prevent HS from worsening, and stop new breakouts. Corticosteroids can also help reduce inflammation, which can help clear HS and prevent new breakouts. Another option for some women is hormone therapy.9 Currently only 1 biologic (adalimumab) has been appoved by FDA and EMA for the treatment of HS.
In some people, HS proves difficult to treat and does not respond to medications. Surgery can be effective in treating people who have had HS for a longer period of time. Surgery is sometimes successful in rendering HS inactive over long periods, though sores may recur.22 For severe cases of HS that do not respond to other treatments, radiation therapy may be an option.4
Many people with HS experience anxiety, depression, and social isolation related to HS symptoms. Psychological symptoms of HS may improve with talk therapy, cognitive behavioral therapy (CBT), meditation, or by engaging with a support group, either in person or on myHSteam.14 If you are feeling depressed, talk with your doctor about treatment. Antidepressant medication may be an effective treatment for some people.
Home remedies and lifestyle changes help some people with HS feel better. Read 5 Ways to be Proactive About HS.
Health Conditions Associated With HS
Aside from hidradenitis suppurativa itself, some of the most common health conditions that occur along with HS include the following:23
- Obesity is considered a risk factor for HS and can exacerbate symptoms.
- Diabetes is more likely in people with HS than people who don't have the skin condition. Obesity is considered a possible factor in that statistic.
- Metabolic syndrome (a combination of high blood glucose, obesity, high cholesterol, and high blood pressure) often occurs along with HS.
- Depression is common in people with HS, as with all chronic conditions. People with HS have a higher rate of suicide than the general population.24 It is just as important for people with HS and depression to seek treatment for their psychological symptoms as it is to treat their skin symptoms.14
- Crohn’s disease and ulcerative colitis seem to have a link with HS.
- Heart disease is more common in those with HS.
- Rheumatoid arthritis and psoriatic arthritis are more common in people with HS.
- Other skin diseases, including open sores on the legs, often occur with HS.
- Skin cancer risk may be higher in those with HS.
To learn more about all of our advanced treatment options for HS, book an appointment online today, or call 866.400.3376. Also, learn more about HS Clinical Trials offered by Ameriderm Research.
REFERENCES
- Wayne Gulliver, Christos C. Zouboulis, Errol Prens, Gregor B. E. Jemec, and Thrasivoulos Tzellos (2016). “Evidence-based approach to the treatment of hidradenitis suppurativa/acne inversa, based on the European guidelines for hidradenitis suppurativa.” National Center for Biotechnology Information, U.S. National Library of Medicine. Retrieved at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5156664/. Accessed May 2019.
- “What Is Hidradenitis Suppurativa?” Hidradenitis Supparativa Foundation. https://www.hs-foundation.org/what-is-hs. Accessed April 2019.
- Lee, R. (1987, 1989, 1999, 2002, 2012). “Hidradenitis Suppurativa,” National Organization for Rare Disorders (NORD). Retrieved at https://rarediseases.org/rare-diseases/hidradenitis-suppurativa/. Accessed May 2019.
- Alikhan, Ali MD, Sayed, Christopher MD (2019). North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations. Journal of the American Academy of Dermatology. Retrieved at https://www.jaad.org/article/S0190-9622(19)30367-6/fulltext. Accessed May 2019.
- “Hidradenitis Suppurativa: Overview.” American Academy of Dermatology Association. https://www.aad.org/public/diseases/painful-skin-joints/hidradenitis-suppurativa
- Dufour, Deirdre Nathalie; Emtestam, Lennart; Jemec, Gregor B (2019). “Hidradenitis suppurativa: a common and burdensome, yet under-recognised, inflammatory skin disease.” BMJ Journals, https://pmj.bmj.com/content/90/1062/216. Accessed May 2019.
- Authored by Armstrong, Walter; Reviewed by H0, Roger S. MD (2017). “The Largest-Ever Epidemiological Study Brings Hidradenitis Suppurativa Into Sharp Focus.” Retrieved at https://www.medpagetoday.com/resource-centers/advances-in-dermatology/largest-ever-epidemiological-study-brings-hidradenitis-suppurativa-into-sharp-focus/1641. Accessed May 2019.
- Saunte DM, Boer J, Stratigos A, et al. Diagnostic delay in hidradenitis suppurativa is a global problem. Br J Dermatol 2015; 173:1546. Retrieved at https://www.uptodate.com/contents/hidradenitis-suppurativa-treatment. Accessed April 2019.
- Lee, Erika Yue MD. “What is hidradenitis suppurativa?” Official Publication of the College of Family Physicians of Canada. Retrieved at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5395382/. Accessed May 2019.
- “Who Gets Hidradenitis Suppurativa?” American Academy of Dermatology Association. https://www.aad.org/public/diseases/painful-skin-joints/hidradenitis-suppurativa#causes. Accessed April 2019.
- Authored by Dr. Harding, Mary; reviewed by Dr. Cox, John (2016). “Hidradenitis Suppurativa.” The Information Standard. Retrieved at https://patient.info/skin-conditions/hidradenitis-suppurativa-leaflet. Accessed April 2019.
- “Hidradenitis Suppurativa.” Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hidradenitis-suppurativa/symptoms-causes/syc-20352306. Accessed May 2019.
- “Hidradenitis Suppurativa: A Treatment Challenge.” American Family Physician. https://www.aafp.org/afp/2005/1015/p1554.html. Accessed May 2019.
- “Mental and Health Support.” Hidradenitis Suppurativa Foundation. https://www.hs-foundation.org/mental-emotional-health. Accessed April 2019.
- Garg, A., Papagermanos, V., Midura, M., & Strunk, A. (2018). Incidence of hidradenitis suppurativa among tobacco smokers: A population-based retrospective analysis in the U.S.A. British Journal of Dermatology,178(3). doi:10.1111/bjd.16391
- Sartorius, K., Emtestam, L., Jemec, G., & Lapins, J. (2009). Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. British Journal of Dermatology,161(4), 831-839. doi:10.1111/j.1365-2133.2009.09198.
- Lee, E. Y., Alhusayen, R., Lansang, P., Shear, N., & Yeung, J. (2017). What is hidradenitis suppurativa?. Canadian family physician Medecin de famille canadien, 63(2), 114–120.
- Khoury, Muin J (2016). “Rare Diseases, Genomics and Public Health: An Expanding Intersection.” Centers for Disease Control and Prevention. Retrieved at https://blogs.cdc.gov/genomics/2016/02/17/rare-diseases/. Accessed May 2019.
- Calao, M., Wilson, J. L., Spelman, L., Billot, L., Rubel, D., Watts, A. D., & Jemec, G. (2018). Hidradenitis Suppurativa (HS) prevalence, demographics and management pathways in Australia: A population-based cross-sectional study. PloS one, 13(7), e0200683. doi:10.1371/journal.pone.0200683
- “The Hurley and Sartorius Systems: Two Methods of Staging.” Consultant 360. https://www.consultant360.com/exclusives/hurley-and-sartorius-systems-two-methods-staging-hs. Accessed May 2019.
- “Hidradenitis Suppurativa.” British Association of Dermatologists http://www.bad.org.uk/for-the-public/patient-information-leaflets/hidradenitis-suppurativa/?showmore=1&returnlink=http%3A%2F%2Fwww.bad.org.uk%2Ffor-the-public%2Fpatient-information-leaflets#.XMzEV-tKjVo. Accessed May 2019.
- Gill, L., Williams, M., & Hamzavi, I. (2014). Update on hidradenitis suppurativa: connecting the tracts. F1000prime reports, 6, 112. doi:10.12703/P6-112
- “Managing Other Health Risks When You Have Suppurativa.” Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hidradenitis-suppurativa/in-depth/managing-other-health-risks-when-you-have-hidradenitis-suppurativa/art-20399321. Accessed April 2019.
- Thorlacus L, Cohen AD, Gisalon GH, et al (2017). “Increased suicide risk in patients with hidradenitis suppurativa.” Journal of Investigative Dermatology. Retrieved at https://www.ncbi.nlm.nih.gov/pubmed/28942360. DOI: 10.1016/j.jid.2017.09.008